There’s no question that dietary changes must happen both pre- and post-surgery. Two nutrients in particular, the mineral calcium and the fat soluble vitamin D, are two very critical nutrients post-surgery. Let’s start with calcium first.
Calcium is an essential nutrient that our bodies need every day; in fact, it’s literally the most abundant mineral in the entire body. The majority of our body’s calcium can be found in structures like bones and teeth, and the remaining is found elsewhere. The “remaining calcium” is so critical that it’s pivotal in growth, maintenance and reproduction, and also plays a big role in muscle contractions, blood clotting hormone secretion and blood pressure homeostasis.
Fun fact: the body heavily regulates what the medical community refers to as, “serum calcium.” What this means is that if the diet is low in calcium, the body will leach it from bones and other stores to maintain proper serum levels.
Around the age of 30 most adults reach peak bone mass, and sufficient calcium intake is crucial to arriving at this point (and staving off conditions like osteopenia, a leading cause of osteoporosis). Consistent and regular calcium intake and physical activity (along with vitamin D, but more on that later) reduces your risk of developing osteoporosis following surgery (and later on in life).
So what happens if we become calcium deficient? Well, nothing too noticeable in the short term. But long term deficiency presents in the following ways:
- Muscle cramps
- Convulsions
- Numbness and tingling in the extremities
- Arrhythmias
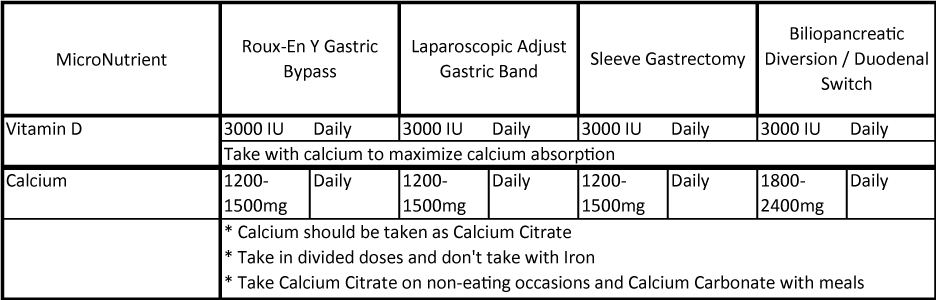
Since symptoms of deficiency are usually delayed, it’s important to listen to your doctor’s guidance on calcium supplementation. The American Society for Metabolic and Bariatric Surgery (ASMBS) has guidance on intake that can range from 1200 mg/day all the way up to 2400 mg/day. Typically, citrated calcium is recommended in divided dosages (not more than 500 – 600 mg at each time as the body best absorbs calcium at these levels). See last section for tips on maximizing calcium absorption.
- No more than 500 – 600 mg citrated calcium per dose.
- Divide it up over at least 3 to 4 occasions.
- Don’t combine calcium with iron supplements or iron-containing multivitamins (separate iron by at least 2 hours).
- Separate calcium doses by at least 2 hours.
- Get your levels regularly checked as to monitor your nutrition status.
Vitamin D is another critical nutrient especially when it comes to maintaining serum calcium levels, as well as actually absorbing both dietary and supplemented calcium. When it comes to what type of Vitamin D, stick with Vitamin D3 (labeled as cholecalciferol).
The vast majority of bariatric patients will require pre-surgical vitamin D supplementation as well as post-surgical supplementation. Why? There are a few major reasons:
- Up to 80% of bariatric patients present with vitamin D deficiency.
- Bariatric surgeries affect nutrient absorption, especially in the small intestine. This affects vitamin D absorption.
- Sufficient vitamin D intake contributes to better calcium absorption.
Therefore, in order to maximize your calcium absorption and prevent long-term deficiencies and health complications, please be sure to do the following:
- Speak with your surgeon and/or dietitian about your current supplement regime.
- Ensure your citrated calcium has vitamin D3 as part of the supplement.
- Do not take calcium along with any iron or iron-containing multivitamins.
- Divide the dose to not more than 500mg calcium per occasion, separated by 2 hours.
- Be mindful of tannin-rich food intake like iced tea, tea, wine and coffee).
- Know your vitamin D status as this optimizes calcium absorption.

